
Regulations mandating adoption of HL7® FHIR® are a major focus for payers in 2024. On January 17, 2024 the Centers for Medicare and Medicaid Services (CMS) issue the Interoperability and Prior Authorization Final Rule (CMS-0057-F), which outlines mandates for payers to streamline health information exchange and prior authorization. The rule builds on the Interoperability and Patient Access Final Rule (CMS-9115-F) and expands FHIR API usage. Complying with these requirements can present challenges, but also offer opportunities to advance innovation with a modern standardized framework for data exchange.
On a December 2023 AHIP webinar, Kendra Obrist from Point of Care Partners and Dr. Russell Leftwich, MD from InterSystems shared their insights for payers interested in strategic approaches to FHIR implementation and innovation. During the discussion, payers were surveyed on their organization’s approach to regulatory compliance as part of their overall enterprise strategy. 33% of those surveyed identified as ‘box checkers’ or ‘cautious followers’ – following the market and doing only what’s necessary to meet compliance standards. 67% identified as ‘strategic positioners’ or ‘leaders and innovators’ – operating with a well-defined strategy, willing to invest in technology, and aligning compliance with long-term goals. Adopting strategies that go beyond ‘checking the box’ of compliance can lead to new approaches in patient care, competitive advantage in the marketplace, and the potential to enable better health outcomes for members.
Where to Start?
Payers who want to seize the opportunity to innovate and differentiate their approach through FHIR implementation will be able to transform current operations, modernize data resources, and maximize innovation opportunities.
Organizations on this path should start by defining an enterprise strategy in three key phases. It’s important to design a comprehensive interoperability approach, instead of letting regulatory compliance requirements and timelines drive every decision.
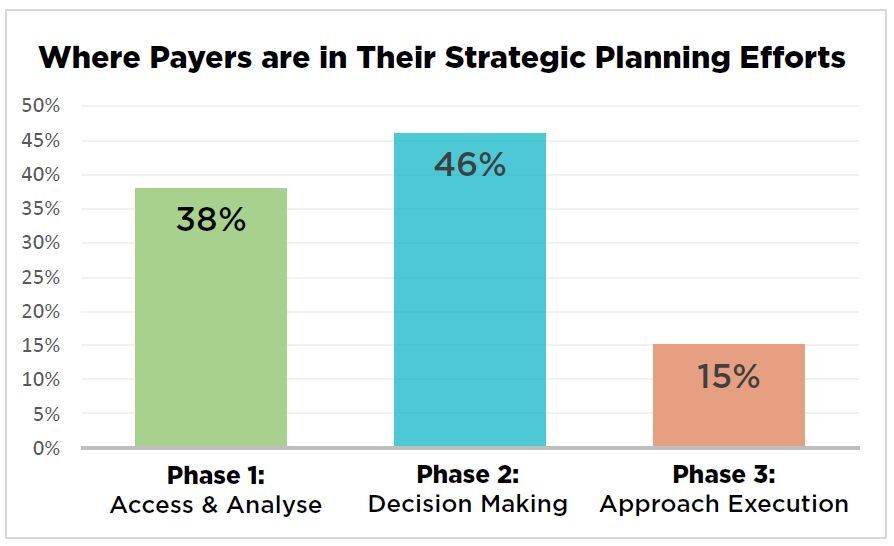
Payers were surveyed on their current efforts, and results revealed many are only in the earliest stages of planning their interoperability approach. When asked where they were in their strategic planning efforts, 38% replied they are in Phase 1, assess and analyze. 46% of respondents are in Phase 2, decision making. Only 15% of those surveyed are in Phase 3, executing their approach.
For payers without a compliance strategy, no time should be wasted in getting started. Reporting elements of the Interoperability and Prior Authorization final rule start in January 2026. Full compliance with the API requirements is required by January 2027, and CMS will release additional detail on enforcement in the future. To meet the regulatory implementation and compliance guidelines, payers should launch strategic planning efforts in early 2024, if they’re not already underway. The assessment and analysis phase should transition into decision-making by late 2024, to allow for a 2025 focus on execution, implementation and testing complex new processes with your business partners. With this timeline, you and your team can also begin to develop and see benefits from innovative strategies that leverage an updated, modernized data infrastructure.
The Transformative Potential of Strategic FHIR Implementation
The new interoperability regulations indicate the intent for payers to own and share the longitudinal data record for their members. A unified view across a member’s health care experiences with different organizations provides a more holistic view of those members. When payers align and strategically invest in their longitudinal data record alongside FHIR API implementation they will unlock opportunities to transform their approaches to managing member health, engaging providers, and measuring outcomes. Payers can learn from initiatives leveraging FHIR APIs aimed at improving patient care and clinical workflows already underway.
- In Rhode Island, a FHIR API has been designed to provide a longitudinal data overview that helps providers more safely manage pain in a population with high opioid use. The Rhode Island Quality Institute uses HIE data to create a single source of actionable information for providers managing patients’ chronic pain.
- In upstate New York, Hixny health information network and Healthy Alliance, a social services provider, have partnered to make it easier for clinicians to assess, track, and treat a patient’s social needs. Hixny’s comprehensive patient record includes a FHIR API that displays a patient’s social and medical history side by side, and enables providers to make referrals. The API creates a recommendation for a social services referral, connects to the local social services network, and ultimately closes the referral loop when Healthy Alliance sends outcome data back to Hixny and the clinician.

When asked if their organization is already using FHIR for projects other than what’s currently mandated by CMS, only 37% said yes. While nearly two-thirds of respondents have not yet started to build FHIR API approaches outside of what’s required, interest in the potential for innovation is strong.
Payers are uniquely positioned to collect and aggregate data because they typically maintain a relationship with individual patients over long periods of time. Making investments to maximize the utility of the longitudinal data record for patients is a prime opportunity for innovation and lasting improvement in health outcomes. Building a strategic approach to interoperability and leveraging internal and external resources will deliver value for years to come and allow payers to make the most of meeting FHIR implementation requirements.
InterSystems supports payers on the path to FHIR implementation. With industry-leading technology, subject matter experts to support implementation, and customized approaches, partnering with our teams will set a foundation for success.


























