Interoperability mandates from the Centers for Medicare and Medicaid Services (CMS) have been a major focus for health plans in recent years and will be critical in informing overall organizational strategies for 2024 and beyond. Yet many organizations look at the efforts they put into the last round of mandates and see little return on investment to date, making them skeptical of the new Interoperability and Prior Authorization rule (CMS-0057-F).
At the HIMSS Global Health Conference & Exhibition in March 2024, InterSystems brought together industry leaders with diverse perspectives to offer their perspectives on how to ensure that regulatory mandates align with payers’ strategic and operational goals. The panel included:
- Dominick Bizzarro, Chief Strategy Officer, MVP Health Care
- Douglas Dietzman, Managing Director, Interoperability Solution, Blue Cross Association
- Jim Adamson, Payer Business Transformation Manager
- Julie Smith, Manager, Product Management, InterSystems
Panelists talked about understanding the direction of regulatory policy and new technological models, and how they align with your goals. They also talked about understanding the rules themselves, and the impact on those you serve. With this understanding, you can, as Bizzarro stated:
MVP Health Care
An Agile Planning Framework for Regulatory Compliance
Bizzarro recommends employing the concepts of Agile Development to the strategic planning process, recognizing that no matter how well researched and deeply informed a 5–10-year strategic plan may be, the reality on the ground will never match what was planned for. An agile approach lets an organization set its overall direction, informed by a variety of factors, including regulatory trends, and then iterate and adjust continuously in the context of an overall vision. He recommends approaching regulatory implementation and compliance from an innovation mindset, and thinking through five key questions:
Five Key Questions
A Framework and Foundation for Innovation
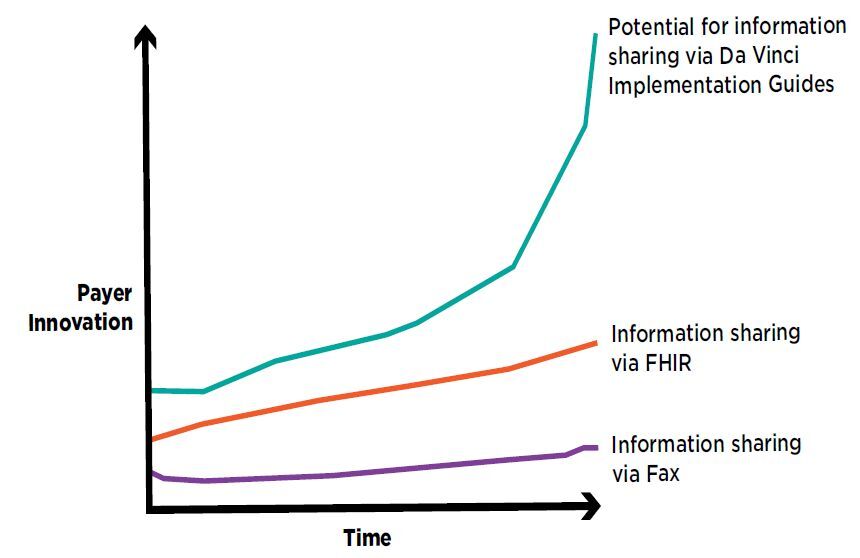
With the HITECH act, CMS and ONC digitized and aligned provider EHR data. CMS-9115-F advanced API-based information sharing for payers. The new CMS-0057-F focuses on advancing interoperability and automating prior authorizations using APIs based on the HL7 Da Vinci Project collaborative work between payers, providers, and vendors. Adamson sees this latest development as particularly significant. He asked the audience to grab a lunch napkin and draw the following:
What is Your Why and How Do the Mandates Help You Get There?
Bizzarro’s first question was about WHY. Adamson told us HOW. Dietzman and Smith brought together the why, the how, and the current regulatory mandate using stories of the human impact of information sharing. Dietzman drew on his deep experience in health information exchange to illustrate the impact that comprehensive health data can have on the individual members of a health plan. Smith brought to the conversation her experience as daughter, mother, nurse, and informatician, to highlight the cost and unnecessary confusion that come with gaps in health records. She then brought the discussion back to the mandate to help us understand HOW it addresses the WHY:
- Payer-to-payer data sharing expands the information set available for individual and plan level decision making.
- Payer-to-provider information sharing helps providers understand the patient in front of them to manage care more effectively.
- Payer-to-patient information sharing that includes prior authorization decisions builds a culture of transparency between members and their health plans.
- Electronic prior authorization uses technology to free up increasingly scarce clinical resources so they can instead invest in managing care.
The key takeaway from the session is that while this new set of mandates will indeed take effort to implement, there is, in fact, tremendous benefit to be gained from doing so. Benefits for providers, for members, and for health plans themselves.

























